
Why use a pulse oximeter?
Oxygen (O2) is transported from the lungs to the cells by the blood. O2 is either fixed to hemoglobin or free in the blood. However, the amount of free O2 in the blood is minimal compared to O2 fixed to hemoglobin, and free O2 does not participate significantly to the total oxygen content in the blood. Therefore, the oxygen content in the blood can be decreased by either decreasing hemoglobin concentration (bleeding, anemia, etc.) or by decreasing the proportion of hemoglobin with O2 fixed. This proportion is called the hemoglobin oxygen saturation in the arterial blood (SpO2).
A pulse oximeter is able to measure SpO2 if the device can detect a pulse. However, it does not assess hemoglobin saturation. This device also calculates heart rate. A photoplethysmographic curve can also be provided on some monitoring devices (see Figure 1). It represents the variation of the diameter of the arteries over time.
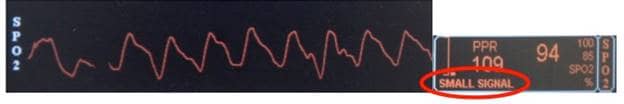 Figure 1: Waveform obtained from the pulse oximeter
Figure 1: Waveform obtained from the pulse oximeter
The box with orange text gives data obtained from the signal analysis, such as heart rate (109) and oxygen saturation (94). Notice the words “small signal” circled in red below the heart rate. It indicates a signal of poor quality even though the waveform looks normal. The amplitude of the waveform does not reflect the quality of the signal as the gain is often adjusted automatically.
Pulse Oximeter Advantages
- Non-invasive
- Quick and easy to use
- Continuous monitoring
- Audible signal
Pulse Oximeter Disadvantages
- Late alert for respiratory problems: hemoglobin is already 100% saturated when breathing room air (21% O2). Therefore, even by increasing the quantity of O2 breath, SpO2 does not go above 100% under anesthesia (100% O2). In this context, SpO2 under anesthesia should not be below 100% unless there is a major respiratory issue (see Figure 2 for explanations).
- Numerous factors can affect the reading, such as pulse quality (vasoconstriction and compression of vessels by the probe), arrhythmia, hemoglobin characteristic (methemoglobin, carboxyhemoglobin, etc.), movement of the patient, skin or mucosa pigmentation, and ambient light. The amplitude of the waveform does not reflect the quality of the signal as the gain is often adjusted automatically; therefore, it should not be used to assess the quality of the signal and data (see Figure 1).
 Figure 2: Hemoglobin dissociation curve
Figure 2: Hemoglobin dissociation curve
The arterial partial pressure of oxygen (PaO2) determines the oxygen saturation of the hemoglobin (SpO2). In-room air, PaO2 is around 100 mmHg, which corresponds to a SpO2 of 100%. Under anesthesia with 100% oxygen, PaO2 should be around 500-600 mmHg, and the SpO2 100%. For the saturation to decrease below 100%, PaO2 needs to be below 100 mmHg, and this would happen only if there was a severe respiratory problem during anesthesia.
When to use a pulse oximeter?
Hypoxemia is one of the common risks under anesthesia. In human medicine, the use of pulse oximeters before anesthesia begins is part of the “surgical safety checklist” designed by the World Health Organization. A pulse oximeter is quick and easy to use; therefore, it should be used for every patient as soon as the level of sedation allows it and should be continued until full recovery. The monitoring of heart rate and saturation as an audible signal is very useful, especially during induction and for high-risk patients (pneumonia, cardiac disease, sepsis, etc.).
A SpO2 below 90% is considered critical for the patient.






